Indianz.Com > News > ‘We just need to be safe’: Monkeypox vaccine rolls out in Indian Country
‘We just need to be safe’: Monkeypox vaccine rolls out in Indian Country
Tuesday, August 23, 2022
Indianz.Com
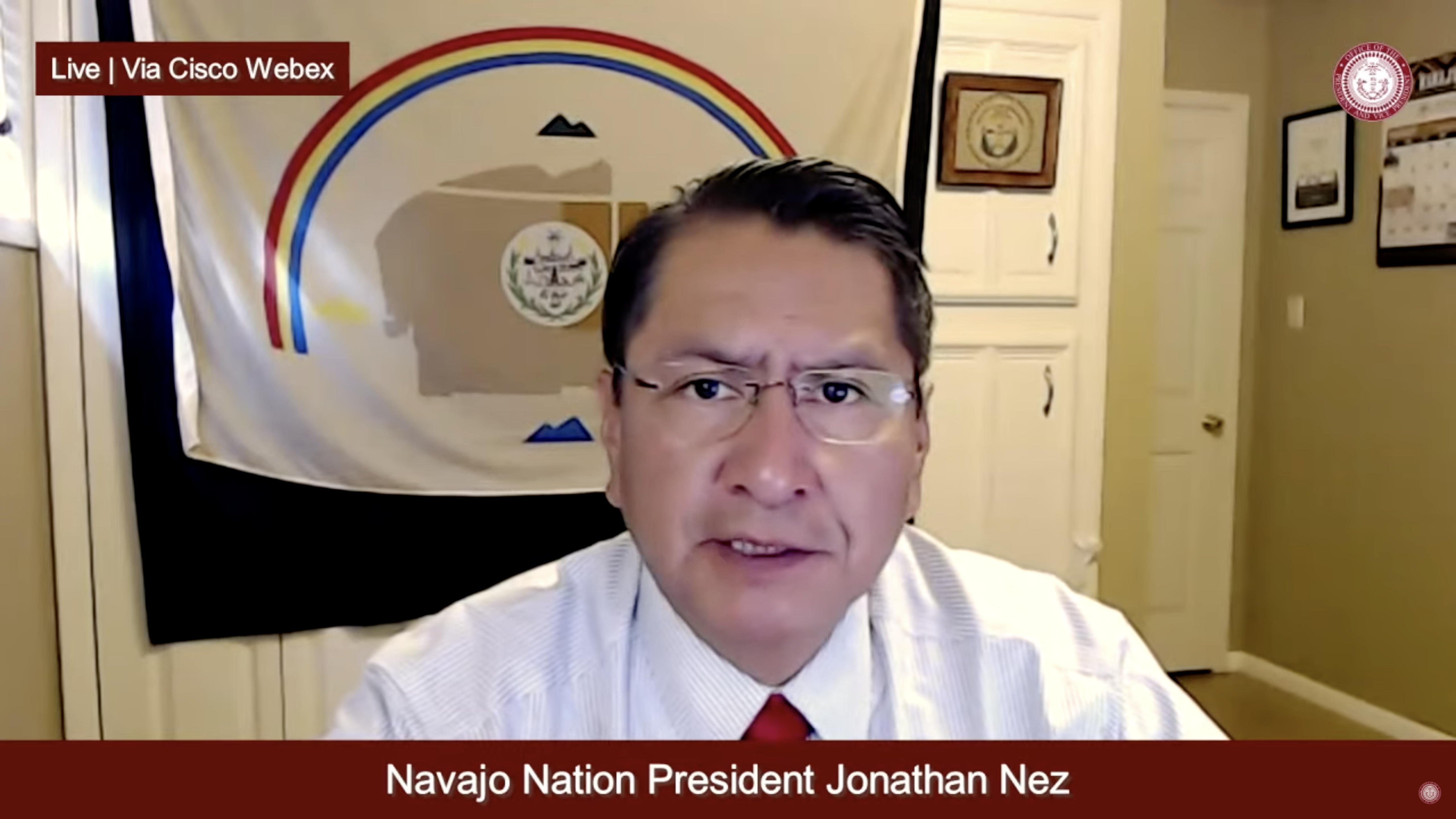
The Navajo Nation is receiving its first doses of the Monkeypox vaccine as experts and providers in Indian Country respond to the latest public health threat.
During a town hall on Tuesday, President Jonathan Nez said his tribe reached out directly to the White House to secure the Monkeypox vaccine doses. The shipment is expected to arrive later in the week.
“I just got word that, this week — Thursday, Friday — we will have the monkeypox vaccination,” Nez said from the largest reservation in the United States.
Nez compared the new effort to his tribe’s response to the ongoing COVID-19 pandemic, which has impacted Navajo people at disproportionate rates. In addition to contacting President Joe Biden, he said a letter was sent to the Department of Health and Human Services, the parent agency of the Indian Health Service.
“Just the same as we did with the vaccine for COVID-19, we advocated heavily,” Nez said of the Navajo Nation’s push to obtain the Monkeypox vaccine.
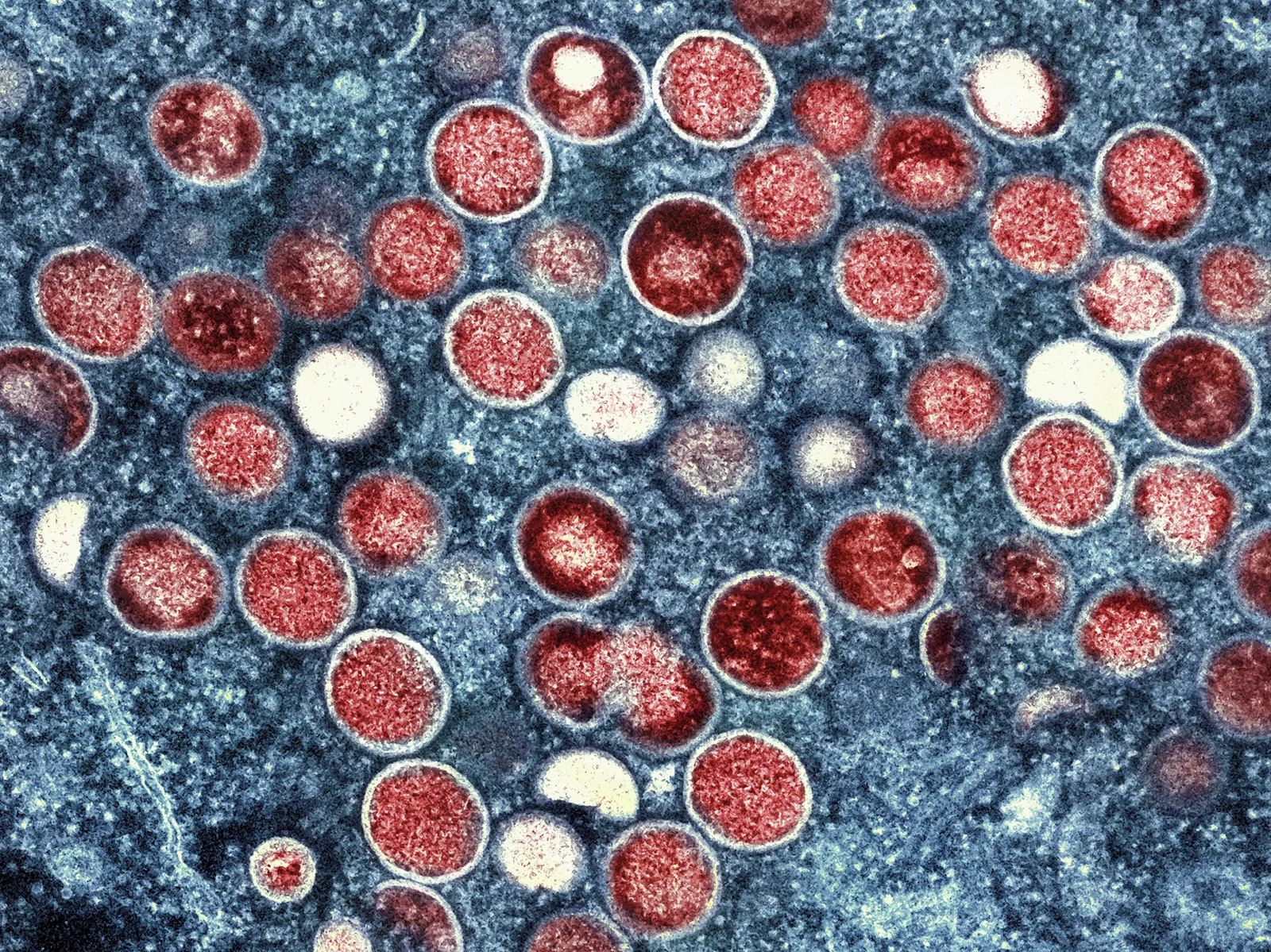
The view from the CDC should become clearer later this week, just as the Navajo Nation receives the Monkeypox vaccine. On Friday, the NIHB is hosting a webinar with representatives of the agency to keep Indian Country informed. The CDC has begun to provide some demographic data for Monkeypox cases among American Indians and Alaska Natives. The very first confirmed cases for Native people appear to have emerged in late June, according to the results. Based on the CDC data, the proportion of Monkeypox cases among Native people is low, when compared to other racial and ethnic groups. But the results are obscured by the fact that American Indians and Alaska Natives represent a little over 1 percent of the overall population in the U.S. Data from jurisdictions with significant Native populations should instead provide a better picture of the impact of Monkeypox in Indian Country. But so far states like Arizona, New Mexico and Oklahoma are referring visitors to the CDC — whose results do not contain a breakdown of cases among American Indians and Alaska Natives. One of the few jurisdictions reporting Monkeypox cases for American Indians and Alaska Natives, as well as Native Hawaiians, is the District of Columbia. As of this week, one Native person — account for 0.3 percent of total cases — was diagnosed with the disease, according to the D.C. Health agency. According to the U.S. Census Bureau, about 1,900 people in the District of Columbia identify as American Indian or Alaska Native, accounting for nearly 0.3 percent of the population. Many are employees of the federal government — the Bureau of Indian Affairs and the National Indian Gaming Commission are headquartered in D.C. Others are employed in the legal field and with several inter-tribal organizations. California is another jurisdiction reporting Monkeypox data among American Indians and Alaska Natives, notable because the state is home to the largest number of Native people. According to the data, seven cases have been reported, accounting for 0.3 percent of the total. Despite the declaration of the national emergency, an official from the IHS told listeners of the Navajo Nation town hall on Tuesday that Monkeypox is a “rare disease” — and one that is rarely fatal. No deaths have been reported in the U.S. since the first cases were reported in May. “The threat of Monkeypox still continues to remain low,” said Brian K. Johnson, who is currently serving as the deputy director of the IHS Navajo Area. “However, it is here,” Johnson added. “We do know that it’s in our surrounding states.” Symptoms of the disease include a rash that can take the form of pimples or blisters in various places of a person’s body, Johnson said. The current outbreak has arisen from “close, sustained physical contact with other people who have Monkeypox,” he added. Such intimate contact has resulted in the rash appearing on and around a person’s mouth, as well as in the genital area, Johnson said. “The good news is that here is vaccines that are effective against this particular virus,” said Johnson, who confirmed that the Navajo Nation will be receiving what is known as the JYNNEOS vaccine. Similar to the COVID-19 vaccine, JYNNEOS is given through a shot in a person’s arm. According to the Food and Drug Administration, two doses are needed, four weeks apart.ANYONE can become infected with monkeypox. Join us on August 26 for the second webinar in our Vaccine Week series! Register at: https://t.co/kljOMNpJPg#NativeHealth #HealthyNativeCommunities #ProjectFirstline #NIHB #COVID-19 #VaccineHesitancy pic.twitter.com/CjQ4LZjjYK
— NIHB (@NIHB1) August 23, 2022
But due to the limited number of doses in the national stockpile, the U.S. currently cannot meet the anticipated demand for JYNNEOS. So the FDA has approved the use of one dose of the Monkeypox vaccine — still delivered via shot, through an “intradermal injection” that will be injected in the upper skin layer of a person’s arm. “Although we don’t have, you know, cases per se here on the Navajo Nation, We know that we’ll have that protective measure of having the JYNNEOS vaccine here on site, which is very, very important for us,” said Johnson. Johnson said the IHS will be working with its own facilities, as well as health care provides operated by the Navajo Nation, to determine how to distribute the Monkeypox vaccine on the reservation. In the U.S., cases have primarily emerged among men who engage in intimate activity with other men — but the NIHB points out that anyone can contract the disease, regardless of age, sex, race, ethnicity or gender. “The providers will be the ones who work with patients and determine who might be at most need of those early vaccinations,” Johnson said of the relationship between the IHS and the Navajo Nation."Our health care professionals strongly encourage everyone to be very cautious with the spread of #COVID19 and now the spread of #Monkeypox": Navajo Nation reports 93 new #Coronavirus cases & 1 death on August 12, 2022. #Arizona #NewMexico #Utah @NNPrezNez https://t.co/wGnws3HlA2
— indianz.com (@indianz) August 15, 2022
Search
Filed Under
Tags
More Headlines
Native America Calling: Can the right approach close the Native immunization gap?
Cronkite News: Long COVID cases remain high in Arizona
Native America Calling: Eyes in the sky for development, public safety, and recreation
Native America Calling: Three new films offer diverse views of Native life
NAFOA: 5 Things You Need to Know this Week
Chuck Hoskin: Cherokee Nation works toward cure for arthritis
Native America Calling: Protecting young people from the down sides of social media
Cronkite News: Fake ‘shaman’ among candidates failing to make Congressional ballot
Native America Calling: New Native voices in poetry
Cronkite News: Tribes air concerns about border at hearing in nation’s capital
Native America Calling: Indiginerds descend on Oklahoma City
Native America Calling: Political leaders target tribes with unfounded claims
Cronkite News: First Native woman in space shares unique journey
Native America Calling: Tackling a troubling trend for Native women in prison
Chuck Hoskin: Cherokee Nation safeguards our Native language
More Headlines
Cronkite News: Long COVID cases remain high in Arizona
Native America Calling: Eyes in the sky for development, public safety, and recreation
Native America Calling: Three new films offer diverse views of Native life
NAFOA: 5 Things You Need to Know this Week
Chuck Hoskin: Cherokee Nation works toward cure for arthritis
Native America Calling: Protecting young people from the down sides of social media
Cronkite News: Fake ‘shaman’ among candidates failing to make Congressional ballot
Native America Calling: New Native voices in poetry
Cronkite News: Tribes air concerns about border at hearing in nation’s capital
Native America Calling: Indiginerds descend on Oklahoma City
Native America Calling: Political leaders target tribes with unfounded claims
Cronkite News: First Native woman in space shares unique journey
Native America Calling: Tackling a troubling trend for Native women in prison
Chuck Hoskin: Cherokee Nation safeguards our Native language
More Headlines